Why Your Tailbone Pain Won’t Let Up (And How to Fix It)
Why Your Tailbone Pain Won’t Let Up (And How to Fix It)
You know that feeling when you plop down on your seat a little too hard, and suddenly your tailbone reminds you it exists? Or when a long car ride turns into a game of “How many different ways can I sit before I lose my mind?” If that sounds familiar, you’re in the right place.
Tailbone pain—also called coccydynia—can be stubborn, making everyday things like sitting, exercising, or even getting up from a chair feel like a battle. But why does it linger for so long? And more importantly, what can you do about it? Let’s break it down and get you on the path to relief.
Understanding Tailbone Pain
Coccydynia is the medical term for tailbone pain, and if you’ve ever experienced it, you know how frustrating it can be. The tailbone (aka the coccyx) sits at the very bottom of your spine and is made up of 3-5 small fused bones. It connects to the sacrum (the triangular bone just above it) at a small joint.
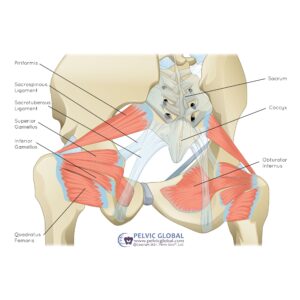
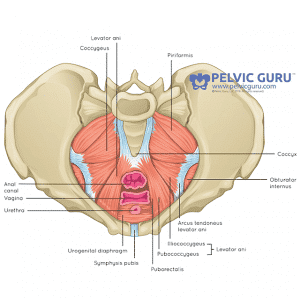
Despite being small, the tailbone has some big responsibilities. It helps with balance and weight distribution when you sit, working alongside your sit bones (the bony parts of your pelvis you feel when sitting on a hard surface). It’s also an attachment point for several important muscles, including parts of the pelvic floor and glutes. These muscles help support bowel, bladder, and sexual function, meaning tailbone issues can sometimes cause discomfort beyond just sitting.
When everything is working well, you probably don’t think twice about your tailbone. But when it’s irritated? Sitting, standing, and even certain movements can become unbearable.
Common Causes
Tailbone pain can come out of nowhere or build up over time, and there are a few common culprits that might be to blame:
1) Trauma
- A backward fall directly onto your tailbone—like slipping on ice or missing a step—can lead to bruising, dislocation, or even a fracture.
- Childbirth, especially if labor was long, required forceps or vacuum assistance, or involved significant pushing, can put a lot of stress on the coccyx.
2) Poor Posture & Sitting Habits
- Sitting for long periods on hard, narrow, or unsupportive surfaces (think bleachers at a sports game, a wooden dining chair, or even a bike seat) can irritate the tailbone over time.
- Slumping or leaning back in a chair, especially with a tucked pelvis, puts extra pressure on the coccyx. If you often find yourself lounging back on the couch or sinking into a soft chair, your tailbone might not be happy about it.
3) Overuse & Muscle Strain
- Strength training without proper form—especially exercises targeting the glutes, hip rotators, or pelvic floor—can strain the muscles around the tailbone. Movements like heavy squats, deadlifts, or even excessive Kegels can contribute to pain if the muscles aren’t engaging properly.
4) Pain Coming from Other Sources
The coccyx itself doesn’t always cause tailbone pain—sometimes, issues in nearby joints and muscles can refer pain to the area. A few common causes include:
- Spinal issues: Problems like degenerative disc disease or arthritis in the lower back or sacrum can create tension and pain that radiates to the tailbone.
- Joint instability: Too much or too little movement at the sacrococcygeal joint (where the tailbone meets the sacrum) or the sacroiliac joints (where the sacrum meets the pelvis) can lead to discomfort. This instability can stem from:
- Arthritis that’s developing in the joints over time
- Pregnancy-related ligament laxity due to the hormone relaxin
- Connective tissue disorders like Ehlers-Danlos Syndrome
- Weakness in the muscles that help stabilize the pelvis and lower back
If any of these sound familiar, don’t worry—there are ways to address tailbone pain and get you sitting comfortably again.
How Tailbone Pain Becomes Chronic
Tailbone pain doesn’t always start suddenly—it can build over time due to posture, muscle imbalances, or underlying dysfunction. Even when there’s an obvious injury, like a fall or childbirth trauma, the pain can linger if the surrounding structures aren’t functioning optimally.
One of the biggest reasons tailbone pain becomes chronic is everyday positioning and posture. Most of us spend a good chunk of our day sitting for work, commuting, or just relaxing. But sitting in nonoptimal positions—like slouching, leaning back onto our tailbones, or sitting for hours without breaks—can keep irritation and inflammation going.
Another often-overlooked cause is pelvic floor muscle dysfunction. If the muscles around the tailbone, including the pelvic floor, become too tight (hypertonic) or imbalanced, they can pull on the coccyx and cause lingering pain. This is something many general healthcare providers don’t routinely assess, meaning the root cause of your pain might go undiagnosed. Seeing a pelvic health therapist can help determine whether muscle tension, rather than a direct injury, is behind your discomfort.
In cases where there’s no clear trauma to the tailbone and imaging doesn’t show an obvious issue, providers may sometimes dismiss the pain or assume it’s unexplainable.
But just because nothing appears on an X-ray or MRI doesn’t mean the pain isn’t real—or that you can do nothing about it!
You’re not alone in this. Many people have felt the same way and found relief through pelvic floor therapy. Here’s a real-life experience from one of our patients:
“I was experiencing extreme tailbone pain and diastasis recti after my first pregnancy. I started going to therapy to be able to sit without having pain. I was given a tailored treatment plan to address all the problems I had (even the ones I didn’t know existed). Everyone on staff was knowledgeable and helpful. I left feeling stable and was able to return to CrossFit again!”
Managing Tailbone Pain at Home
Dealing with tailbone pain can be challenging, but you can try several at-home strategies to find relief. Here are some tips that can make a difference:
Posture:
- Sit up straight! Your spine should be aligned, not rounded. Keep your feet flat on the floor and avoid slouching or leaning back too much. A slight forward lean can help.
- Ensure your back and pelvis are aligned against the back of your chair.
- Engage your abdominal muscles gently to support your back.
- Distribute your weight evenly between your butt cheeks—try not to lean to one side.
Cushions:
- Your chair should be soft and supportive. Consider using a cushion that alleviates pressure on the tailbone. Some cushions even have a cutout designed for this purpose. Here’s a helpful option!
Heat and Cold Therapy:
- Applying a heating pad or ice pack to your tailbone can provide temporary relief. Use whichever feels best for you! However, be cautious about switching between hot and cold—too much can lead to increased sensitivity. Also, avoid overusing the heating pad to prevent skin irritation.
Self-Massage and Stretching:
- Try rolling a tennis ball gently over the muscles around your tailbone to relieve tension.
- While lying on your side, lift the top gluteal muscle away from your tailbone—you should feel a good stretch!
- Here are some stretches that can help with pelvic floor muscles:
- Child’s Pose
- Happy Baby
- Deep Squat
- Diaphragmatic Breathing
Modify Daily Activities:
- Make it a habit to get up every hour to relieve pressure on your tailbone.
- Try adjusting how you get in and out of the car to minimize discomfort.
- Use a supportive cushion while sitting or driving, and consider cushions with cutouts to reduce pressure on the tailbone.
Prevent Muscle Tension:
- Stretch regularly to keep your muscles from getting too tense.
- Pay attention to your bowel habits. Hard stools can put extra pressure on your tailbone, so it’s important to maintain a healthy diet. You can find more about dietary habits in our digestive blog post and tips for better bowel movements in our toileting techniques blog post HERE
With these tips, you can take active steps to manage your tailbone pain at home. Remember, small changes can make a big difference!
The Role of Pelvic Floor Therapy in Managing Tailbone Pain
If you’re struggling with tailbone pain (coccydynia), a specialized pelvic floor therapist can help identify the root cause and develop a personalized treatment plan. Unlike general practitioners, pelvic floor therapists take a comprehensive look at not just your coccyx but also the surrounding structures to understand how they work together as a system. Your pain may stem from pelvic floor dysfunction, muscle imbalances, joint mobility issues, or problems in your back or pelvis. Here’s how a pelvic floor therapist can support you:
Comprehensive Assessment:
Your therapist will start by conducting a thorough evaluation to pinpoint the cause of your tailbone pain. This may involve examining your back, pelvis, and coccyx and, in some cases, a gentle internal or external pelvic floor examination. Based on this assessment, your therapist will create a customized care plan tailored to your needs.
Relaxation Techniques:
To help relax tight muscles, your therapist may teach you various stretches, breathing techniques, and mindfulness strategies. These techniques can be particularly beneficial if you’re experiencing hypertonic (tight) muscles. You can learn more about this in our hypertonic blog post HERE
Manual Therapy:
Your therapist may use hands-on techniques, such as myofascial release, trigger point release, or joint mobilization, to relieve muscle tension and improve joint mobility. Depending on your needs, these methods can be applied to areas like the pelvic floor, coccyx, pelvis, back, or hips. Additionally, your therapist might introduce tools like a pelvic wand and guide you in using them effectively.
Neuromuscular Re-education:
Learning to properly coordinate and activate your pelvic floor muscles, along with surrounding muscles like your abdominals and glutes, is essential. This process helps create a balanced muscle use pattern and relieves strain on overworked areas. Mastering this coordination will lay the groundwork for strengthening exercises.
Strengthening Exercises:
Building strength in your core muscles—including your abdomen, back, hips, and pelvic floor—can significantly enhance your overall function. This foundation will prepare you for more challenging exercises, activities, and sports.
Lifestyle Modifications:
Your therapist can help you identify daily habits or postures that might be contributing to your tailbone pain, providing suggestions for adjustments that can lead to better outcomes.
Collaborative Care:
Sometimes, managing tailbone pain requires a team effort. Your therapist may collaborate with other specialists, such as gynecologists, urologists, orthopedists, or chiropractors, to address underlying factors like stress, posture, or related conditions.

Core and hip strength go hand in hand! Our therapist is helping this patient properly engage her muscles and build stability using the Pilates reformer without adding tension to her lower back. Exercise is possible, EVEN if you are having pain/discomfort!
Working with a pelvic floor therapist can provide valuable insights and tools for effectively managing tailbone pain and improving one’s quality of life.
How to Advocate for the Care You Need
Navigating your healthcare journey can feel overwhelming, especially when dealing with persistent tailbone pain. Here are some helpful tips and questions to guide your conversations with your physical therapist (PT) and doctor:
Questions to Ask Your PT and Doctor:
- Understanding the Cause: Don’t hesitate to ask your provider what they believe is causing your pain and how their suggested treatment approach is designed to address it.
- Exploring Specialized Care: If your tailbone pain isn’t improving—especially after trying medical interventions or standard orthopedic physical therapy—consider having an open discussion about the possibility of getting a referral to a specialized pelvic floor therapist.
When to Consider Seeing a Doctor for Imaging Tests:
- Acute Pain After Injury: If your tailbone pain appears suddenly and severely after a specific event (like a fall), imaging to check for potential fractures is essential.
- Worsening Symptoms: If your pain is getting worse quickly, or if you start feeling symptoms radiating down your legs or into your spine, imaging can help rule out other underlying causes.
FAQ
“Why does my tailbone hurt when I sit for long periods?”
The tailbone, or coccyx, supports and stabilizes the body while sitting and bears much of the weight. Prolonged sitting can exert a lot of force and pressure on the tailbone, leading to discomfort and pain. For instance, if you work at a desk for hours without taking breaks, you might notice this pain becoming more pronounced.
“Is there anything I should avoid doing while suffering from coccyx pain?”
Yes, certain activities can exacerbate tailbone pain, including:
- Sitting for long periods: Try to take regular breaks to stand or stretch.
- Sitting on hard or narrow surfaces: Opt for cushioned chairs or seats with cutouts for the tailbone.
- Sitting with poor posture: Maintain a straight spine and avoid slouching.
- Cycling: Traditional bike seats can be uncomfortable. If cycling is essential for you, consider a wider or more cushioned seat.
- Getting constipated: Strain during bowel movements can put extra pressure on your tailbone.
- Stress that causes increased muscle tension: Managing stress through relaxation techniques can help alleviate muscle tension around the tailbone.
“Why do I have tailbone pain postpartum if I didn’t have a birth injury?”
Even if you didn’t experience a birth injury, several factors can contribute to postpartum tailbone pain:
- Tailbone Movement During Delivery: The tailbone tilts backward to allow the baby to descend through the vaginal canal, leading to increased movement and potential strain.
- Pelvic Floor Muscle Changes: During vaginal delivery, pelvic floor muscles stretch significantly, which can create abnormal pulling on the tailbone. This tension may not resolve on its own after delivery, and the muscles might tighten as they heal, contributing to ongoing pain.
- Weight Changes: The tailbone bears additional weight and downward pressure throughout pregnancy. Postpartum, it may need to be readjusted to a new weight and pressure management, causing discomfort.
“How long does it typically take for tailbone pain to heal?”
The healing time can vary based on the root cause of your pain, how long it has persisted, and its severity. Generally, treatment for tailbone pain takes anywhere from 8 to 20 weeks, especially with consistent weekly therapy sessions.
“Will my tailbone pain affect my sexual health and intimacy?”
Possibly. Penetrative intercourse can increase pressure on the tailbone, particularly in positions where the tailbone doesn’t have room to move. To mitigate discomfort, try different positions that don’t put direct pressure on the tailbone, such as side-lying or using pillows for support.
Additionally, if your tailbone pain is linked to pelvic floor muscle hypertonicity (tightness), this can also affect intimacy. When pelvic floor muscles are hypertonic, they may not stretch and lengthen properly during intercourse, leading to friction and discomfort.
Wrapping It Up
In conclusion, tailbone pain can be challenging, but understanding its causes and exploring effective management strategies can lead to relief and a more comfortable life. Whether you’re utilizing at-home strategies, seeking support from a specialized pelvic floor therapist, or advocating for the care you need, remember that you’re not alone in this journey. Taking proactive steps can make a significant difference in your healing process. Prioritize your pelvic health, and don’t hesitate to reach out for the support you deserve. You’ve got this!
Contact Us
Have questions or want to learn more about how physical therapy can help you enjoy intimacy again? Reach out—UpLift is here to guide you through your pelvic floor journey!