From Surgery to Strength: Navigating Your Tummy Tuck Recovery
From Surgery to Strength: Navigating Your Tummy Tuck Recovery
So, you’re thinking about a tummy tuck (abdominoplasty)—or maybe you’ve already had one. You’ve done the research, chosen your surgeon, and planned for the big day. But what happens after surgery? Recovery is more than just waiting for time to pass—it’s about moving smart, managing swelling, and rebuilding strength in a way that supports your body.
As a physical therapist specializing in lymphedema and post-surgical rehab, I work with people recovering from procedures like tummy tucks all the time. This guide will walk you through the healing process with practical tips to help you regain strength and get back to doing what you love—safely and confidently.
What Happens During a Tummy Tuck (Abdominoplasty)?
A tummy tuck, or abdominoplasty, is a surgical procedure that removes excess skin and fat from the abdomen while also tightening the underlying muscles. It’s often chosen by individuals who have experienced significant weight loss, pregnancy, or age-related changes that lead to loose skin and weakened core muscles.
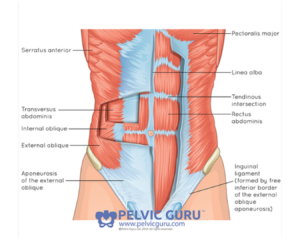
Your abdominal muscles play a crucial role in posture, movement, and recovery. Here’s a closer look at their structure.
There are different types of tummy tucks, ranging from mini to full abdominoplasty, depending on how much skin and muscle repair is needed. While the procedure is sometimes cosmetic, it can also have functional benefits, such as improving core stability and posture, especially for those with severe diastasis recti (a separation of the abdominal muscles).
What to Expect After Surgery
Let’s walk through what recovery looks like in the first few days and weeks after surgery—and why having the right support can make all the difference.
The First Few Days: Managing Swelling & Discomfort
Right after surgery, your body’s number one priority is healing. Swelling, bruising, and discomfort are completely normal, but knowing what to expect can make the process feel less overwhelming.
Here’s what you’ll likely experience:
Swelling & Fluid Retention – Your lymphatic system will be working hard to clear excess fluid from the surgical area. Swelling may fluctuate throughout the day, which is completely normal.
Incision Care – Following your surgeon’s protocol for cleaning and managing your incisions is key. This also means avoiding lifting or strenuous activities to allow optimal healing. You may need to adjust your clothing, sleep position, and daily activities to stay comfortable.
Limited Mobility – Standing fully upright might be tough at first due to tightness in your abdomen. Small, frequent movements will be your best friend.
Drains & Compression Garments – Many tummy tuck procedures involve surgical drains to remove excess fluid (unless your surgeon specializes in drain-less techniques). You’ll likely also wear a compression garment to help reduce swelling and support healing tissues.
Early Recovery Tips
-
- Gentle Movement Is Key
- Short, frequent walks around your home can help prevent stiffness and reduce the risk of blood clots.
- Lymphatic Drainage Can Help
- A trained therapist can perform manual lymphatic drainage (MLD) to encourage fluid movement and reduce swelling. Early visits can optimize healing and speed up recovery.
- Support Your Scar Healing
- Keeping incisions clean and following your surgeon’s scar care guidelines can help reduce tension and improve healing.
- Pain Management Matters
- Talk to your surgeon about your pain management plan to stay as comfortable as possible while allowing your body to heal.
- Work With a Specialist
- A trained rehab therapist can guide you through safe mobility, monitor incision healing, and communicate with your surgeon if needed. You’ll also want to plan for transportation to and from appointments since driving won’t be an option at first.
- Gentle Movement Is Key
Other Tips to Make Your Recovery Easier
-
- Have a few soft, button-up shirts on hand for easy dressing.
- Stock up on easy-to-prepare meals or premade options to avoid heavy cooking and overhead lifting.
- Plan for comfortable sleep—recliners, wedges, bolsters, and lots of pillows can help.
- Keep essentials within easy reach (below shoulder height) to minimize unnecessary strain.
Weeks 2-4: Moving Toward Strength & Stability
By the second and third weeks post-op, you’ll likely start feeling better—but swelling and fatigue can still be present. Many people are eager to return to daily activities, but this phase is where strategic recovery becomes crucial.
Common Challenges During This Stage
-
- Persistent Swelling – Some swelling is still expected, but if you notice one-sided swelling, increased pain, or hard lumps, reach out to your healthcare team to rule out any concerns.
- Core Weakness – Your abdominal muscles were stretched and tightened during surgery, so it’s normal to feel weaker through your core. This can impact posture, balance, and movement.
- Tissue Tightness & Scar Adhesions – The incision area may feel tight or even “stuck.” Gentle mobility exercises, scar massage (once cleared by your surgeon), and working with a therapist can help restore movement and flexibility.
- Energy Levels & Fatigue – Even though you’re feeling better, your body is still healing, and fatigue can hit unexpectedly. Overdoing it too soon can slow recovery.
- Postural Changes & Back Discomfort – Since standing fully upright may still feel unnatural; some people experience back strain from compensating. Gentle stretching and mindful posture adjustments can help.
- Emotional Ups & Downs – The healing process isn’t just physical. Some people experience frustration with recovery speed, temporary body changes, or post-surgical blues. Support from loved ones (or even a professional) can be helpful.
Strengthening After a Tummy Tuck: A Safe & Smart Approach
Recovering from a tummy tuck isn’t just about letting your incision heal—it’s about gradually rebuilding strength, mobility, and core function. While you might be eager to return to exercise, jumping in too soon (or doing the wrong movements) can put stress on healing tissues and slow your progress.
Let’s go over when it’s safe to start moving again, which core exercises to avoid early on, and how gentle stretching and walking can support your recovery.

Gentle movement, breathwork, and stretching can aid in post-surgical healing. A pelvic PT can help you regain strength safely.
When Can You Start Reintroducing Light Activity?
Healing timelines vary based on the type of tummy tuck you had and your overall health, but here’s a general guide:
Weeks 1-2: Rest & Light Walking
-
- Focus on short, gentle walks (5-10 minutes at a time) to promote circulation and prevent stiffness.
- Avoid lifting, bending, or any movement that engages your core—your muscles are still healing.
- Listen to your body and rest when needed.
- Try mild postural exercises, like backward shoulder rolls and gentle shoulder blade squeezes, to prevent tension buildup.
Weeks 3-4: Gradual Increase in Movement
-
- Continue walking and slightly increase the duration if it feels comfortable.
- Introduce gentle stretching (avoiding deep abdominal stretches).
- Light, functional movements, like transitioning from sitting to standing with good posture, help reintroduce safe core engagement.
Weeks 6-8: Light Strength Training & Mobility Work
-
- Most surgeons clear patients for light bodyweight exercises and controlled core activation around this time but always follow your personal clearance timeline.
- A physical therapist can guide you in safely reintroducing movement without unnecessary strain.
- Start breathing and pelvic floor re-connection exercises to gradually rebuild core stability.
Weeks 8-12: Gradual Core Strengthening
-
- Safely begin low-intensity core engagement, such as deep breathing exercises, pelvic tilts, and modified core work.
- Increase walking duration and consider adding gentle incline walking.
- Introduce mobility work to optimize core function and posture.
Always get clearance from your surgeon before increasing activity levels!
Core Exercises & Movements to Avoid Early On
Protecting your abdominal muscles is crucial in the early stages of healing. During the first 6-8 weeks, avoid movements such as:
- ❌ Traditional Core Exercises – Sit-ups, crunches, planks, leg raises, and Russian twists create too much pressure on healing tissues.
- ❌ Heavy Lifting – Avoid lifting anything over 10 lbs to prevent strain.
- ❌ Twisting & Deep Bending – Movements like bicycle crunches and deep forward folds can overstretch healing tissues.
- ❌ High-Impact Activities – Running, jumping, and intense cardio can increase swelling and stress on the incision.
The reason for avoiding these movements is that they can place excessive strain on your core and may be risky without guidance from your surgeon or physical therapist. Ensuring your body has fully healed before reintroducing these exercises will protect your recovery and minimize the risk of complications.
How Working With a Physical Therapist Can Help
A lymphedema or post-surgical physical therapist can be a crucial part of your recovery journey. Here’s how they can support you:
Teach Safe Scar Mobilization – Gentle, hands-on techniques can help prevent scar tissue from becoming stiff or restricting movement, allowing you to regain flexibility and comfort as you heal.
Guide Core Activation – Post-tummy tuck, not all abdominal exercises are appropriate. A therapist can introduce safe, low-impact movements that help reconnect you with your deep core, ensuring you’re activating muscles without overloading them.
Assist with Lymphatic Drainage – If swelling persists, a physical therapist trained in manual lymphatic drainage (MLD) can use specialized techniques to encourage fluid movement, reduce swelling, and improve comfort, speeding up the recovery process.

Cupping is one of many techniques pelvic PTs use to improve scar mobility, reduce tightness, and support recovery.
Long-Term Healing: Returning to Full Strength
By the one-month mark, many people start feeling significantly better, but remember, full recovery can take several months. Swelling may still come and go, and your body is continuing to adjust. This stage is all about laying the groundwork for a smooth recovery and focusing on the following:
Gradual Strength Building – A physical therapist can guide you as you transition from light mobility exercises to more functional strength training, which supports your posture, movement patterns, and core stability.
Scar & Tissue Flexibility – Gentle soft tissue techniques can help improve the flexibility and mobility around your incision site, ensuring it moves freely as you continue healing.
Listening to Your Body – Some days you’ll feel amazing, and other days, swelling may reappear. Recovery isn’t always linear, and that’s completely normal. It’s important to honor your body’s signals and adjust as needed to support your healing journey.
FAQs
“How long will it take to get back to CrossFit/the gym after my tummy tuck?”
This really depends on how well you’re healing. Most people start to feel ready for gentle exercises around 4 months post-surgery. More intense activities, like CrossFit or high-impact workouts, may take longer. It’s important to work with a trained professional to safely transition back into these activities and avoid pushing your body too soon.
“How does recovery differ for men versus women?”
The healing process is pretty similar for both men and women, but individual health factors play a big role. The key to a smoother recovery is optimizing your health going in—managing blood sugar if you’re diabetic, increasing protein intake, and avoiding smoking or alcohol while healing. Your overall wellness will impact how well you recover.
“If I had a tummy tuck without muscle repair, will my recovery be easier?”
In some ways, yes. If you didn’t require muscle repair, you might be able to reconnect with your core more quickly. However, your recovery will still depend heavily on how well your incisions heal and how effectively you manage swelling. Extra swelling can delay muscle activation, so be sure to follow your care team’s guidance closely.
“When can I start doing ab exercises after my surgery?”
This varies based on your unique healing timeline. It’s important to wait until you get clearance from your surgeon or physical therapist, and even then, start with gentle movements before progressing to more intense ab exercises.
“How can I prevent developing complications during tummy tuck recovery?”
Working with a trained rehabilitation professional and staying in close contact with your surgeon are key to preventing complications. Professional guidance ensures you’re moving through recovery safely, addressing any issues early, and optimizing healing.
“How long do I have to wear my compression garments?”
The timeline for wearing compression garments depends on your surgeon’s specific protocol. Generally, they’re a vital part of managing swelling, and you’ll likely need to wear them for at least the first 2 months. Your surgeon will guide you on when it’s safe to stop wearing them.
Final Thoughts: Investing in a Supported Recovery

Rebuilding core strength after surgery takes time. A pelvic PT can guide you through controlled, safe exercises to support recovery.
Tummy tuck recovery goes beyond just resting—it’s all about active healing. Managing swelling, restoring movement, and rebuilding strength are essential steps in the process. This procedure can offer both aesthetic and functional benefits, transforming not only your appearance but also your overall well-being.
Healing comes first, and strength follows. By working with a trained professional, you can ease into movement with walking, gentle stretching, and gradual core engagement, rebuilding strength safely without putting healing tissues at risk.
Whether you’re preparing for surgery or navigating the early stages of recovery, it’s valuable to work with someone who specializes in post-surgical healing, lymphatic health, and core rehabilitation. A physical therapist trained in lymphedema and post-op recovery can support you in moving through the process with confidence and ease.
Contact Us
Have questions or want to learn more about how physical therapy can aid in your tummy tuck recovery? Reach out—UpLift is here to guide you through the healing journey!

