Navigating Pelvic Organ Prolapse: Your Guide to Causes, Symptoms and Solutions
Navigating Pelvic Organ Prolapse: Your Guide to Causes, Symptoms & Solutions
Pelvic organ prolapse (POP) affects many people, yet it remains one of those topics often left in the shadows. Whether you’re new to this diagnosis, experiencing symptoms, or just curious, understanding what pelvic organ prolapse is can be empowering. In this blog, we’ll break down what prolapse means, explore common symptoms, and dive into the range of treatment options, from conservative therapies to surgical interventions. You’ll also find guidance on when to seek help, tips for living well with prolapse, and insights into managing symptoms for a healthier, more comfortable life.
What is Pelvic Organ Prolapse?
Pelvic organ prolapse occurs when organs in the pelvic region—like the bladder, uterus, rectum, or small intestine—shift from their usual positions and press into the vaginal canal. This condition is most commonly caused by a weakening of the pelvic floor muscles and connective tissue, which can no longer provide adequate support to the pelvic organs.
Common causes include:
- Pregnancy and vaginal childbirth
- Aging and menopause
- Obesity
- Chronic coughing or straining (e.g., during bowel movements)
- Past pelvic surgeries (such as a hysterectomy)
- Genetics and certain connective tissue disorders (like Ehlers-Danlos syndrome)
- Improper heavy lifting over time
Types of Prolapse
Pelvic organ prolapse isn’t a one-size-fits-all condition. It can involve one or more pelvic organs shifting from their normal positions. Here are the main types:
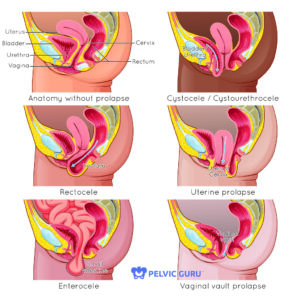
Pelvic organ prolapse explained! This diagram breaks down rectocele, cystocele, and uterine prolapse with a side-by-side comparison of healthy anatomy. Knowledge is power when it comes to your pelvic health. The image was used with permission from Pelvic Guru®, LLC, as a member of the Global Pelvic Health Alliance Membership (GPHAM).
1) Bladder Prolapse (Cystocele)
- Description: In bladder prolapse, the bladder drops from its usual position and pushes against the vaginal wall.
- Symptoms: This often results in feelings of heaviness or bulging in the vagina, urinary incontinence, or difficulty with bladder emptying.
2) Uterine Prolapse
- Description: Uterine prolapse occurs when the uterus descends into or even out of the vaginal canal.
- Symptoms: Symptoms can include a sensation of fullness in the lower abdomen, lower back pain, or even visible tissue at the vaginal opening in more severe cases. Many individuals report an increase in symptoms when standing for long periods.
3) Rectal Prolapse (Rectocele)
- Description: A rectocele involves the rectum pressing into the back wall of the vagina.
- Symptoms: People with a rectocele may experience constipation, difficulty with bowel movements, or the need to apply pressure to the vaginal wall to have a bowel movement.
4. Small Intestine Prolapse (Enterocele)
- Description: This type occurs when the small intestine slips down, pressing into the vaginal canal.
- Symptoms: Enterocele is typically associated with lower abdominal or pelvic pressure and discomfort, especially when standing for extended periods.
Each type of prolapse can impact people differently, and it’s also possible to experience multiple types simultaneously. This is known as a multi-compartment prolapse, where more than one organ shifts from its normal position. Please refer to the image below to see how types of prolapse differ.
Symptoms of Pelvic Organ Prolapse
The symptoms of pelvic organ prolapse vary depending on the organs affected and the severity of the prolapse. Common symptoms include:
-
- Vaginal Bulge or Protrusion: A noticeable bulge or feeling of tissue in the vaginal canal.
- Pelvic Pressure or Heaviness: Sensation of pressure that can worsen with prolonged standing or during activities like coughing.
- Lower Back Pain: General ache or discomfort in the lower back.
- Discomfort During Intercourse: Pain, pressure, or a sensation of hitting something internally during sex.
- Urinary Symptoms: Issues such as incontinence, urgency, frequency, or weak urine stream.
- Bowel Symptoms: Constipation, straining, incomplete emptying, or the need to manually shift tissues to pass stool.
Disclaimer: This list of symptoms is not exhaustive, and experiences with pelvic organ prolapse can vary widely. If you have questions or concerns about your symptoms, consult a healthcare provider for personalized guidance.
When to Seek Help

Comfort and consent are our priority. Here, our therapist explains the process of an internal examination to check for potential prolapse, ensuring the patient feels informed and empowered every step of the way.
If you’re experiencing symptoms like a persistent feeling of heaviness or pressure in the pelvis, a visible bulge or protrusion in the vaginal area, urinary incontinence, or discomfort during daily activities, it may be time to reach out to a healthcare provider. These symptoms can affect your quality of life and might not improve on their own, so seeking help can provide both relief and strategies to manage or even prevent further progression.
Early intervention can be key in addressing prolapse effectively. A pelvic floor physical therapist, urogynecologist, or gynecologist can assess your unique symptoms and recommend a treatment plan tailored to your needs.
It’s especially important to consult a professional if your symptoms disrupt your ability to work, exercise, or engage in personal activities, as this could indicate a more advanced stage of prolapse. The sooner you seek support, the more options are likely available to help you live more comfortably and confidently!
Treatment Options for Pelvic Organ Prolapse
Treatment for pelvic organ prolapse can range from conservative management to surgical options, depending on the severity of symptoms and personal health considerations.
1. Pessary
A pessary is a medical device that’s inserted into the vagina to support prolapsed organs and relieve symptoms like pressure and discomfort. Pessaries come in various shapes and sizes and must be fitted by a healthcare provider, such as a pelvic floor physical therapist or gynecologist. Although a pessary doesn’t correct the prolapse, it can significantly improve quality of life and allow for more comfortable physical activity. See the image below for a visual of how pessaries are inserted.
Note: For best results, pessary use is often combined with pelvic floor physical therapy to strengthen and support weakened muscles.

A pessary can make a big difference in pelvic organ prolapse! This diagram shows how a pessary supports the pelvic floor, relieving pressure and reducing discomfort. The image was used with permission from Pelvic Guru®, LLC, as a member of the Global Pelvic Health Alliance Membership (GPHAM).
2. Hormone Therapy
For some individuals, hormonal shifts (especially a decrease in estrogen during menopause) contribute to pelvic organ prolapse. Hormone therapy options include:
- Oral Hormone Replacement Therapy: Systemic hormone therapy can help rejuvenate pelvic tissues and counteract atrophy, though it affects the entire body and may not be suitable for everyone.
- Topical Estrogen Cream: Applied directly to the vaginal tissues, this low-dose option helps revitalize and strengthen local tissue without systemic effects, as it doesn’t enter the bloodstream.
Note: Please discuss these options with a physician to determine if they’re appropriate for your specific needs.
3. Pelvic Floor Physical Therapy
Pelvic floor physical therapy (PFPT) focuses on strengthening and coordinating pelvic floor muscles, which can alleviate prolapse symptoms and improve muscle function over time. Treatment may include:
- Strengthening and coordination exercises for the pelvic floor muscles
- Education on posture and body mechanics to reduce prolapse strain
- Recommendations on prolapse-safe exercises and activities
- Pessary fitting or recommendations, if needed
Unlike basic Kegel exercises, pelvic floor therapy involves a comprehensive assessment and personalized treatment plan, making it highly effective in both treating and managing prolapse symptoms.
4. Surgical Options
In cases where conservative treatments don’t provide relief, surgery may be considered. Surgical options vary depending on the prolapse type and severity and may include:
- Use of mesh or sutures to lift and support prolapsed organs
- Reconstruction techniques, such as using existing pelvic ligaments for support
- Vaginal wall reinforcement or closure (colpocleisis)
- Hysterectomy if the uterus is affected
Note: Surgery should be discussed with a urogynecologist or a pelvic floor specialist who can explain the benefits, risks, and recovery process tailored to your individual case.
Prognosis & Living with Prolapse

Yes, you can lift safely with prolapse! Our therapist is guiding this patient through proper lifting mechanics to protect her pelvic floor and prevent symptom progression. Empowerment starts with education and technique.
Living with pelvic organ prolapse can be difficult, both physically and emotionally. It’s not uncommon for people with prolapse to experience discomfort, frustration, and even embarrassment related to their symptoms, especially as daily activities, exercise, and intimacy can be impacted. This condition can also come with feelings of isolation or self-consciousness, as pelvic health issues aren’t often discussed openly.
The good news is that prolapse is manageable, and many people are able to live fulfilling, active lives with the right combination of treatments. Conservative options like pelvic floor physical therapy and pessaries can significantly reduce symptoms, prevent the prolapse from worsening, and, in many cases, help avoid surgery. Therapies and exercises focus on strengthening and coordinating the pelvic floor muscles, which can relieve symptoms and provide better long-term support for the pelvic organs. For those who do choose surgery, advancements in techniques allow for more customized and minimally invasive options that can offer lasting relief.
It’s important to seek help from a qualified healthcare provider, as the journey of managing prolapse is unique to each individual. Working with a team—including your pelvic floor physical therapist, gynecologist, or urogynecologist—can ensure that your treatment plan aligns with your goals, lifestyle, and specific needs.
Remember, there are many paths to managing pelvic organ prolapse, and with proper care, you can find ways to live confidently and comfortably.
Contact Us
UpLift Physical Therapy Website
Phone: 210-468-7398
Follow us on social media: Instagram @upliftptp